Foodborne disease outbreaks
Consumers expect hygienically safe food and the food industry attaches great importance to the quality of its products. If people nevertheless fall ill as a result of eating food contaminated with pathogens, an attempt should be made to find out the causes.
In individual cases, it is usually not possible to find the cause of the disease in the variety of foods consumed. However, in group illnesses, known as foodborne outbreaks, there is a better chance of finding the food that served as the transmission vehicle for the pathogen by working out characteristic similarities between cases.
Definition: a foodborne outbreak is defined in the Zoonoses Act 2005 as follows: The occurrence, under given circumstances, of a disease and/or infection associated or likely to be associated with the same food or food business in at least two cases in humans, or a situation in which the cases detected are more prevalent than expected.
Situation 2024
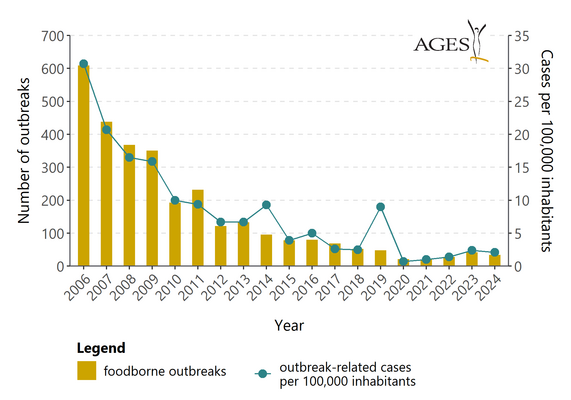
A total of 34 foodborne outbreaks were reported in 2024, 8 fewer than in 2023. In total, 194 people were affected by the outbreaks, a similar number to 2023 (222 people), but significantly fewer than in 2019 (793 people) in pre-coronavirus times. 77 people had to be hospitalised in connection with the outbreaks (2023: 38, 2022: 57, 2021: 27, 2020: 17, 2019: 159); there were two deaths (2023: 1 death, 2022: 4 deaths, 2021: 2 deaths, 2020: no deaths, 2019: one death). The average number of people per outbreak was 5.7 and affected between two and 28 people in each outbreak.
The number of general outbreaks in 2024 (including three international outbreaks and two outbreaks that lasted from 2023) was 18 (53%), the number of household outbreaks was 10 (29%) and there were also six outbreaks of unknown status.
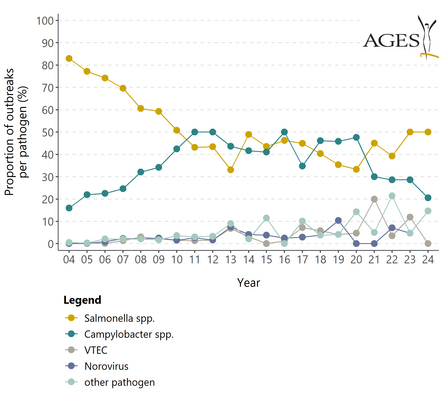
Salmonella was the most common outbreak agent (17 outbreaks, 118 people affected, one death). Campylobacter was in second place (7 outbreaks, 16 cases), followed by five outbreaks caused by norovirus (46 people) and one outbreak each caused by non-typified E. coli (three people), Listeria monocytogenes (four people, one death), Yersinia enterocolitica (two cases), Shigella flexneri (two cases) and hepatitis A virus (three cases).
An important outbreak with strong evidence was a transnational outbreak caused by Salmonella Strathcona ST2559 CT3910 and affected 24 people (4 hospitalisations) already in 2023. This outbreak continues in 2024 and 26 people were involved in Austria. A total of 232 cases occurred in 16 EU/EEA countries and the UK. The suspected foodstuffs were cherry tomatoes from a farm in Italy(European Centre for Disease Prevention and Control, European Food Safety Authority, 2024. Prolonged multi-country outbreak of Salmonella Strathcona ST2559 possibly linked to consumption of tomatoes - 12 November 2024).
A second important outbreak with strong evidence was a Europe-wide outbreak caused by Salmonella Umbilo ST 2014 CT 24675, which resulted in 20 infected persons (2 hospitalisations) in Austria. In total, over 200 cases occurred in various European member states. The contaminated foods wererocket salad and baby spinach from a producer in Italy(Multinational investigation of a Salmonella Umbilo outbreak reveals rocket salad and baby spinach as the likely infection vehicles, Europe, 2024).
In 2024, a general foodborne outbreak with strong evidence - caused by L. monocytogenes Sg IIa/ST101/CT7699 - was reported to the EMS in Austria: four people were affected, all had to be hospitalised and one person died. The foodstuffs responsible were contaminated meat products. One person had already contracted the disease in 2023.
A particularly high number of outbreaks in 2024 were associated with stays abroad (8 outbreaks caused by Salmonella, 1 outbreak caused by Campylobacter and 1 outbreak caused by Shigella flexneri).
| Year | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | 2020 | 2021 | 2022 | 2023 | 2024 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Food-borne outbreaks | 609 | 438 | 368 | 351 | 193 | 232 | 122 | 133 | 96 | 78 | 80 | 69 | 52 | 48 | 21 | 20 | 28 | 42 | 34 |
| - of which due to salmonella | 452 | 305 | 223 | 208 | 98 | 100 | 53 | 44 | 47 | 34 | 37 | 31 | 21 | 17 | 7 | 9 | 11 | 21 | 17 |
| - of which due to Campylobacter7 | 137 | 108 | 118 | 120 | 82 | 116 | 61 | 58 | 40 | 32 | 40 | 24 | 24 | 22 | 10 | 6 | 8 | 12 | 7 |
| Number of cases (in connection with foodborne outbreaks) | 2.530 | 1.715 | 1.376 | 1.330 | 838 | 789 | 561 | 568 | 790 | 333 | 436 | 227 | 222 | 793 | 67 | 92 | 128 | 222 | 194 |
| - Infected persons per 100,000 inhabitants in connection with outbreaks | 30,7 | 20,7 | 16,5 | 15,9 | 10,0 | 9,4 | 6,7 | 6,7 | 9,3 | 3,9 | 5,0 | 2,6 | 2,5 | 9,0 | 0,7 | 1,0 | 1,4 | 2,4 | 2,1 |
| - of which treated in hospital | 493 | 286 | 338 | 223 | 155 | 179 | 97 | 108 | 121 | 86 | 68 | 56 | 58 | 159 | 17 | 27 | 57 | 38 | 77 |
| - Number of deaths | 3 | 1 | 0 | 6 | 2 | 0 | 0 | 0 | 1 | 0 | 0 | 2 | 0 | 1 | 0 | 2 | 4 | 1 | 2 |
Types outbreaks
Based on the Austrian Zoonoses Act, we collect outbreak data annually and forward it to the EU. Certain classifications result for this reporting: Outbreaks in which only members of a single household are affected are categorized as a household outbreak. If individuals from multiple households are affected, this is counted as a general outbreak. Household outbreaks account for the majority (approximately 75%) each year because it is often not possible to epidemiologically link cases of illness from different household outbreaks by identifying a single causative food.
Outbreak clarification
The aim of the outbreak survey is not only to stop the outbreak that is currently taking place, but above all to prevent such diseases in general in the future.
Detailed and systematic searches can succeed in locating both the infectious vehicle, that is, the food that transmitted the infectious agent to humans, and the reservoir, which is the habitat in which an infectious agent normally lives. Only then is it possible to set targeted and meaningful interventions. These measures should result in the elimination of the outbreak cause, namely the infectious agent, from the food chain and consumers are no longer exposed to this agent.
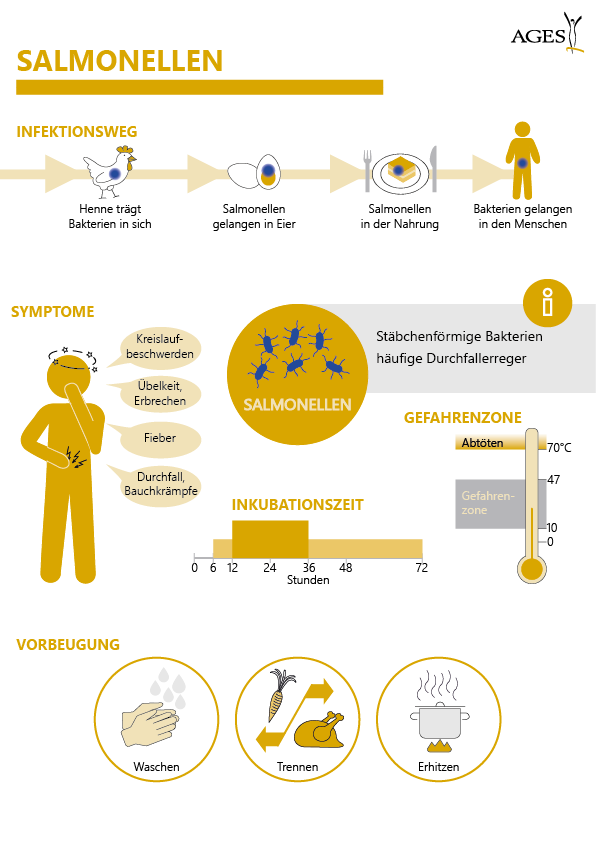
The following historical example illustrates the preventive medical potential of an outbreak investigation: In July 2004, it was possible to clarify a foodborne outbreak caused by Salmonella Enteritidis phage type 36, a very rare Salmonella type in Austria, which affected 38 people in four provinces, and trace it back to a flock of laying hens. The flock was eradicated, the farm thoroughly cleaned and disinfected; subsequently, new laying hens were housed. As a result of these measures, not a single further case of illness caused by Salmonella Enteritidis phage type 36 has been reported in Austria since then.
Since 2009, bacterial and viral foodborne infections and poisonings have been reported via the EMS, an area-wide surveillance system. However, these reporting figures must be viewed in a nuanced manner: Numerous factors can lead to an underestimation of the actual illness figures ("underdetection/underreporting"). Depending on the pathogen, the data situation often varies: for salmonella, for example, data are available from Europe-wide baseline studies, surveillance and control programs. The decrease in salmonellosis cases is an effect of measures implemented on the basis of these data. Toxoplasmosis, on the other hand, is not reportable, although new scientific evidence suggests a link with food. All of these factors must be considered when assessing the true public health significance of a disease.
Implementation
In accordance with the provisions of the Epidemic Diseases Act, the locally competent district administrative authorities must, through the public health officers at their disposal, immediately initiate the surveys and investigations required to identify the disease and the source of infection in the event of any report or suspicion of the occurrence of a notifiable disease - and thus also in the case of foodborne outbreaks. In addition, the Zoonoses Act 2005 obliges the respective competent authorities to investigate foodborne disease outbreaks and, as far as possible, to conduct appropriate epidemiological and microbiological investigations in the process.
In doing so, the authorities have the option to call in experts. Simply stepping up untargeted food sampling has repeatedly proven to be ineffective in the past. In many outbreaks, the causal food (or the affected contaminated batch of the causal product) is no longer available for microbiological investigations at the time of the surveys.
In these cases, an epidemiological study can provide insights that enable preventive measures to be taken to avoid similar incidents in the future. The lessons learned from successfully cleared national and international outbreaks in recent years have put the necessity and usefulness of epidemiological clarifications beyond question.
Thematic report on foodborne infectious diseases 2016
Many authorities and institutions from different areas of expertise are involved in monitoring the food chain. Due to the complexity and the sometimes differing objectives, a comprehensive, joint approach is absolutely necessary. The 4th report in the AGES Wissen Aktuell series,"Foodborne Infectious Diseases", provides this overview. It also describes the causes that can lead to the contamination of animal foods with certain pathogens and the measures that can be taken by both producers and consumers to reduce this.
In Austria, around 8,000 foodborne diseases are recorded in the national epidemiological reporting system (EMS) every year. According to the WHO definition, infectious diseases caused by food are "diseases of an infectious or toxic nature that can actually or probably be traced back to the consumption of food or water".
A total of over 250 pathogens and toxins are known to cause such diseases. This report is limited to 20 pathogens that are of significance in Austria (Campylobacter, Clostridium difficile, EHEC/VTEC, Listeria, Salmonella, Shigella, Vibrio, Yersinia, Noroviruses, Rotaviruses, Sapoviruses, Saponoviruses, Saprotoxins, Saprotoxins, Saprotoxins, Saprotoxins, Saprotoxins, Saprotoxins, Saprotoxins, Saprotoxins, Saprotoxins, rotaviruses, sapoviruses, hepatitis viruses, Cryptosporidium parvum, Toxoplasma gondii, Cyclospora cayetanensis, Giardia and the toxin producers Staphyloccus aureus, Bacillus cereus, Clostridium botulinum, Clostridium perfringens). Pathogens that are virtually absent in Austria or only occur as travellers' diseases were not included.
Last updated: 11.07.2025
automatically translated